Welcoming a new baby into your life is a profound and beautiful experience. However, it also comes with many questions and concerns, especially regarding infant vaccinations. One of the first vaccines any newborn typically receives is the hepatitis B vaccine. If you are a new or expectant parent, you have likely heard about the hepatitis B vaccine for newborns, but you may still have questions about what it does, why it is necessary, and how safe it is.
In this 2025 guide, we will explore the purpose, schedule, safety profile, and benefits of the neonatal hepatitis B vaccine. By the end, you will have a comprehensive understanding of why the newborn hepatitis B vaccine is widely recommended and how it can protect your baby from a lifetime of potential liver complications.
What Is the Hepatitis B Vaccine?
The hepatitis B vaccine (HepB) is an immunization designed to protect against the hepatitis B virus (HBV). This virus infects the liver and can cause both acute and chronic illnesses. In some individuals, HBV leads to lifelong liver conditions, including cirrhosis and liver cancer. Because HBV can be transmitted through blood and other bodily fluids, it is highly contagious even with brief contact.
Key Facts About the Hepatitis B Vaccine:
- Composition: Most versions of the vaccine contain an inactivated form of the hepatitis B surface antigen (HBsAg), produced in yeast cells. This process ensures that the vaccine does not contain a live virus. Therefore, it cannot cause hepatitis B infection.
- Administration: The vaccine is commonly administered as a series of three doses, although certain premature newborns may require four doses depending on their birth weight and maternal HBV status.
- Combined Formulas: In some instances, the hepatitis B vaccine may be part of a combination vaccine that also protects against diphtheria, tetanus, pertussis, polio, or other diseases.
Because hepatitis B virus is prevalent worldwide, health authorities recommend starting vaccination strategies as early as the day of birth. Evidence shows that early vaccination can drastically reduce the likelihood of developing chronic HBV infection.
Why Does a Newborn Need the Hepatitis B Vaccine?
A primary concern for many parents is, “Why do babies get Hep B at birth?” or “Why does a newborn need the hep b vaccine if they are not at high risk?” Even if you have tested negative for HBV, newborns still benefit significantly from receiving the hep b shot at birth:
- Preventing Perinatal Transmission: If a birthing parent carries HBV, the virus can be passed to the infant during or after delivery. Administering the vaccine (and in some cases, hepatitis B immune globulin, or HBIG) within the first 12 hours of life can reduce the baby’s infection risk by a substantial margin.
- Silent Infection Concerns: Hepatitis B is sometimes called a “silent epidemic” because many infected individuals have no symptoms. It’s possible an infected person does not realize they are a carrier and inadvertently transmits HBV through the smallest amount of blood contact or bodily fluid. Risks of skipping the hep b vaccine include missing this crucial chance to protect newborns early in life.
- Lowering Long-Term Liver Disease Risks: Chronic hepatitis B infections lead to significantly higher risks of liver cirrhosis, liver cancer, and other complications. Infants who contract HBV from birth have a high risk of developing chronic infection, which might result in serious illnesses later in life.
- Ease of Prevention: Because the hep b vaccine is both safe and effective, and because newborns are already receiving standard newborn care in a hospital setting, it is practical and beneficial to administer the first dose as early as possible.
The purpose of the neonatal hepatitis B vaccine is to give your baby immediate armor against an infection that can be difficult to detect and treat. By taking proactive steps at birth, you can help your child avoid persistent health risks down the road.
How the Vaccine Protects Newborns
The infant hep b vaccine teaches the immune system to recognize and fight the hepatitis B virus without ever exposing the child to the active infection. Once injected, the inactive HBsAg protein triggers the body’s natural immune response. The body then develops antibodies specifically targeted against HBV.
Key Mechanisms of Protection:
- Antibody Production: Upon receiving the vaccine, a baby’s immune cells produce antibodies that attach to any recognized hepatitis B viral surface proteins in the bloodstream and neutralize them.
- Immunological Memory: After vaccination, the infant’s immune system “remembers” HBV. Should the child later encounter the actual virus, the body rapidly mounts a defensive response before infection can take hold.
- Long-Term Effectiveness: Research has shown that immunizing infants at birth can provide extended and potentially lifelong immunity for most individuals. While boosters are not routinely recommended for healthy children and teens, certain at-risk groups may require periodic testing or re-vaccination in adulthood.
Hepatitis B Transmission Risks in Infants
Hepatitis B spreads through contact with blood or bodily fluids from an infected person. Even casual exposure to microscopic amounts can be enough to transmit the disease, making it especially worrisome in settings where multiple family members or caregivers come into contact with the infant.
Main Transmission Routes for Infants Include:
- Contact During Birth: The highest risk occurs if the mother (or birthing parent) carries HBV at delivery. Infants in this situation can receive both HBIG and the vaccine within 12 hours of birth to maximize protection.
- Household Exposure: Another layer of hidden risk arises from household transmission. Whether through shared toothbrushes, nail clippers, or small scrapes that come in contact with infected blood, hepatitis B can be unintentionally passed to a baby.
- Day-to-Day Interactions: Although less common, the virus can also be present in saliva and other fluids if blood is mixed in. Babies frequently put things in their mouths and can have minor open scrapes or abrasions, so even minimal virus exposure can lead to infection if they are unvaccinated.
Eliminating the potential for infection is nearly impossible because many people with chronic HBV do not exhibit symptoms. That’s why universal vaccination programs and schedules are recommended—to provide consistent, widespread protection that doesn’t rely on perfect knowledge of everyone’s HBV status.
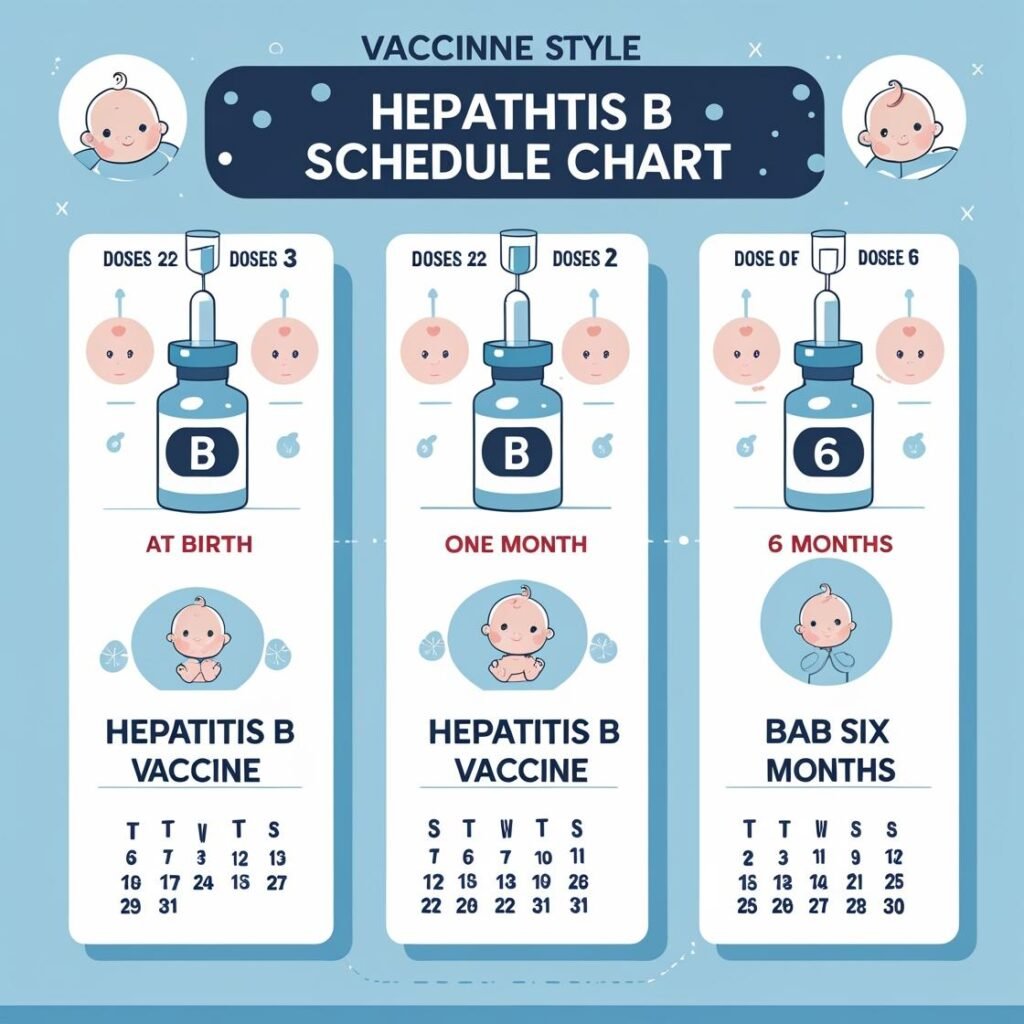
Hepatitis B Vaccine Schedule for Infants (0–18 Months)
According to updated guidelines as of 2025, the hepatitis B vaccine schedule for infants typically consists of three doses (sometimes four, depending on birth weight and maternal HBV status). This ensures that each infant has multiple opportunities to respond to the vaccine and develop robust immunity.
Here is the general recommended schedule:
- Birth Dose
- Given within 24 hours of life. If the mother is HBV-positive, the baby will receive the birth dose within 12 hours, along with HBIG for immediate passive protection.
- If the mother tests negative and the baby’s birth weight is ≥2,000 grams, the dose can be given before hospital discharge or at birth.
- For very low birth weight babies (<2,000 grams) born to HBV-negative mothers, the first dose is usually delayed until the baby is 1 month old or at hospital discharge if earlier.
- Second Dose
- Given around 1–2 months of age. Some combination vaccines containing hepatitis B are also given at 2 months, along with other routine immunizations such as DTaP and Hib.
- Third Dose
- Usually administered at 6–18 months of age. By spacing out these doses, the immune system receives repeated opportunities to learn and solidify its defenses against HBV.
- The last dose should not be given before 24 weeks of age, ensuring the immune system has had enough time between doses to mount a strong and lasting response.
If a baby is born prematurely and has a low birth weight (<2,000 grams), a fourth dose may be added to ensure adequate protection. The exact schedule can vary according to the hospital’s protocols and doctor’s advice.
Before You Go Further…
Before diving deep into the schedule and safety of the Hepatitis B vaccine, make sure you’re keeping track of all your baby’s vaccinations. Use our free Newborn Vaccination Reminder Tool to generate a personalized vaccine schedule based on your baby’s birth date.
What Happens If a Baby Misses the Hep B Vaccine?
Life as a new parent can be hectic. Occasionally, vaccines may be delayed due to illness or scheduling conflicts. If your baby misses a dose of the hepatitis B vaccine series:
- Discuss With a Pediatrician: The most crucial step is to talk with your child’s healthcare provider about catch-up immunizations. Pediatricians are used to adjusting vaccine schedules for a variety of reasons. They can advise you on the best time to administer the missed dose(s) so your child’s protection remains optimal.
- No Need to Restart the Entire Series: Generally, if a baby misses a dose, you do not need to restart the entire hepatitis B vaccine series. Instead, you pick up where you left off, following the recommended intervals between doses.
- Possible Additional Doses: In some rare cases, if there have been significant gaps, the healthcare provider might recommend additional doses to ensure your baby produces adequate antibodies to the virus.
- Risks of Skipping the Vaccine: Delaying or skipping does leave your child unprotected for a longer period, which can increase their susceptibility to infection if exposed. Therefore, catching up as soon as possible is always advisable.
Is the Hepatitis B Vaccine Safe for Newborns?
A top question among new parents is: “Is hep b vaccine safe for newborns?” The short answer is yes. Health authorities worldwide, including the CDC, the American Academy of Pediatrics (AAP), and the World Health Organization (WHO), endorse the hep b shot for newborns as safe and effective when administered according to recommended guidelines.
Safety Highlights:
- Extensive Testing: Before receiving approval for infant use, the hepatitis B vaccine for newborns undergoes rigorous clinical trials and safety evaluations.
- Well-Tolerated: Side effects, if any, are typically mild, including slight soreness at the injection site or low-grade fever.
- No Live Virus: The vaccine contains only a small, harmless component of HBV’s surface protein, so it cannot cause hepatitis B infection.
- Ongoing Monitoring: Vaccine safety is continuously monitored by organizations like the CDC’s reporting systems. Any sign of significant unexpected reactions triggers further investigation.
Rare Side Effects: Although exceedingly rare, anaphylaxis (a severe allergic reaction) can occur at a very low rate. In such cases, medical staff are trained to respond immediately.
Can You Refuse the Hep B Vaccine at Birth?
In the United States and many other countries, vaccines, including the hep b vaccine for infants, are highly encouraged but generally not forced. Parents or guardians often have the legal option to refuse or delay mandatory vaccines for newborns, depending on their local regulations. Hence, the question arises: “Can you refuse the hep b vaccine at birth?”
- Legal Rights: Yes, in many places, parents have the right to refuse. However, they may be required to sign a form that acknowledges they understand the risks of skipping or delaying the vaccine.
- Hospital Policies: Some hospitals have policies to strongly advocate for the birth dose of the hepatitis B vaccine, especially if the parent’s HBV status is unknown or positive. Healthcare professionals might emphasize the significance of immediate vaccination to protect the newborn.
- Potential Consequences: Refusing the vaccine leaves the newborn without this critical protection. If an unvaccinated baby later comes into contact with an infected individual, the risk of contracting the infection rises considerably.
Decisions about vaccination can be challenging. Having a thoughtful conversation with your healthcare provider can help you explore any specific concerns and talk through the exact risks and benefits based on your situation.
When Did the Hepatitis B Vaccine Become Mandatory at Birth?
A common question among parents is, “When did the hepatitis B vaccine become mandatory at birth?”
- U.S. Recommendations: The universal recommendation for hepatitis B vaccination at birth in the United States began in 1991, when public health authorities realized that targeting only high-risk groups did not sufficiently curb HBV infection rates.
- Modern-Day Policies: Over the decades, research and global health efforts have reinforced this recommendation, emphasizing a birth dose for all infants. By 2025, it is standard practice in most hospitals in the U.S. and is strongly encouraged worldwide by agencies like WHO.
Legally, “mandatory” can vary between states or countries in terms of school or daycare entry requirements. Nonetheless, medical experts overwhelmingly endorse the vaccine because of the severe risks to newborns if exposed to hepatitis B without immunity.
Does the Hep B Vaccine Leave a Scar?
In past generations, some vaccines — such as the smallpox or Bacillus Calmette–Guérin (BCG) shots — often left a permanent scar on the arm or shoulder. This visible mark can be seen on the upper arm of many adults and grandparents. However:
- Hepatitis B Vaccine and Scarring: Typically, the hepatitis B vaccine does not leave a scar. Injection site reactions are usually limited to minor redness or swelling, which fades in a few days.
- What Vaccine Left a Scar on Your Arm? The older smallpox vaccine commonly left a round scar on the upper arm. BCG (commonly used against tuberculosis in certain countries) can also do the same. These are different from the hep b vaccine and should not be confused.
If you notice any unusual or persistent mark at your baby’s vaccine injection site, consult your pediatrician to ensure there is no infection or other issue.
Long-Term Health Benefits of Early Immunization
The long-term health benefits of early immunization against hepatitis B span far beyond infancy:
- Reduced Chronic Carrier State: When babies receive the newborn hepatitis b vaccine, they have a significantly decreased chance of developing chronic HBV infection, which can lead to reduced risks of cirrhosis and liver cancer.
- Community Protection: Widespread infant vaccination gradually reduces the pool of active carriers in the population. As more people are vaccinated, fewer will contract and transmit the disease, approaching what experts call “herd immunity” for hepatitis B.
- Boost to Other Vaccines: Administering the hep b vaccine alongside other recommended immunizations ensures that infants can be protected from multiple diseases in their early, most vulnerable stages of life. This organized schedule helps build a strong foundation for a healthy childhood.
- Protection Throughout Adolescence and Beyond: Studies have shown that most children who receive the primary hepatitis B vaccination series do not require later boosters because of robust, long-lasting protection. While some may need to verify immunity through blood tests in adulthood, the majority remain protected for decades.
Providing newborns with the hepatitis B vaccine sets the stage for fewer hepatitis B cases, fewer chronic liver illnesses, and fewer medical complications. It is a simple but powerful intervention.
Frequently Asked Questions (FAQ)

Do newborns really need the Hep B vaccine?
Yes. The goal is to protect infants before they are discharged home, where they could be exposed to carriers of the hepatitis B virus. Since many carriers are unaware of their status, immunizing right away reduces the risk that a baby will become infected during their most vulnerable early months.
What happens if a baby doesn’t get the Hep B vaccine?
If a baby does not receive the neonatal hepatitis b vaccine, they remain susceptible to any potential exposure. Because hepatitis B can spread through insignificant amounts of blood or bodily fluids, an unvaccinated baby is at higher risk for infection, which could lead to chronic hepatitis B, cirrhosis, or even liver cancer in the long term.
Why do babies have HepB at birth?
Healthcare providers administer the hep b shot for newborns to prevent perinatal transmission and to safeguard the child against casual household or community exposures. This immediate protection is critical, given that more than 90% of infants who contract hepatitis B at birth can develop chronic HBV.
When did the hepatitis B vaccine become mandatory at birth?
Routine recommendations for universal newborn hepatitis B vaccination were adopted in the early 1990s. The approach was expanded to include all newborns because targeted vaccination of only high-risk groups did not sufficiently reduce infections in the community. By 2025, this is a recognized global standard recommended by agencies like the CDC and WHO.
Can you refuse the Hep B vaccine at birth?
Generally, yes, parents can refuse the vaccine in certain jurisdictions. However, healthcare experts strongly advise against refusal due to the high risk of chronic infection, cirrhosis, and liver cancer if the baby becomes infected. Talk to your pediatrician about any concerns before making a decision.
What vaccine left a scar on your arm?
The smallpox vaccine is well-known for leaving a scar on the upper arm. Another vaccine called BCG, used primarily in countries with a high prevalence of tuberculosis, can also leave a distinctive scar. Hepatitis B vaccines do not typically cause scarring.
Why Does a Newborn Need the Hepatitis B Vaccine?
Newborns receive the hep b vaccine to protect against an infection that can be silently transmitted and result in serious, lifelong complications. Early vaccination drastically cuts the chances of chronic HBV infection and associated liver diseases later in life.
Final Thoughts
Understanding the hepatitis b vaccine for newborns can spare a lot of anxiety about the vaccination process. As of 2025, robust clinical evidence has underscored the vaccine’s efficacy, safety, and significance in preventing long-term liver problems caused by hepatitis B.
Here are the key takeaways from this guide:
- Immediate Protection: The birth dose provides crucial early defense against any casual or perinatal exposure.
- Safe and Well-Studied: Yes, the hepatitis B vaccine is both safe and protective for newborns.
- Minimal Side Effects: Common reactions include mild discomfort or fever at the injection site. Serious reactions are exceedingly rare.
- Long-Term Security: Vaccinated infants have a reduced risk of liver disease, cirrhosis, and cancer in adulthood.
- Public Health Impact: Infant immunization dramatically reduces the community reservoir of HBV, bringing society closer to potentially eradicating a once-pervasive virus.
If you have any lingering questions about the hepatitis b vaccine schedule for infants, or if your child has missed a dose, it’s best to consult directly with your pediatrician. They can provide guidance tailored to your child’s health status and ensure they remain protected. By embracing early immunization, you are taking a valuable step toward safeguarding your newborn’s health—both now and for decades to come.
